Background: Ivermectin has demonstrated different mechanisms of action that potentially protect from both coronavirus disease 2019 (COVID-19) infection and COVID-19-related comorbidities. Based on the studies suggesting efficacy in prophylaxis combined with the known safety profile of ivermectin, a citywide prevention program using ivermectin for COVID-19 was implemented in Itajaí, a southern city in Brazil in the state of Santa Catarina. The objective of this study was to evaluate the impact of regular ivermectin use on subsequent COVID-19 infection and mortality rates.
Materials and methods: We analyzed data from a prospective, observational study of the citywide COVID-19 prevention with ivermectin program, which was conducted between July 2020 and December 2020 in Itajaí, Brazil. Study design, institutional review board approval, and analysis of registry data occurred after completion of the program. The program consisted of inviting the entire population of Itajaí to a medical visit to enroll in the program and to compile baseline, personal, demographic, and medical information. In the absence of contraindications, ivermectin was offered as an optional treatment to be taken for two consecutive days every 15 days at a dose of 0.2 mg/kg/day. In cases where a participating citizen of Itajaí became ill with COVID-19, they were recommended not to use ivermectin or any other medication in early outpatient treatment. Clinical outcomes of infection, hospitalization, and death were automatically reported and entered into the registry in real time. Study analysis consisted of comparing ivermectin users with non-users using cohorts of infected patients propensity score-matched by age, sex, and comorbidities. COVID-19 infection and mortality rates were analyzed with and without the use of propensity score matching (PSM).
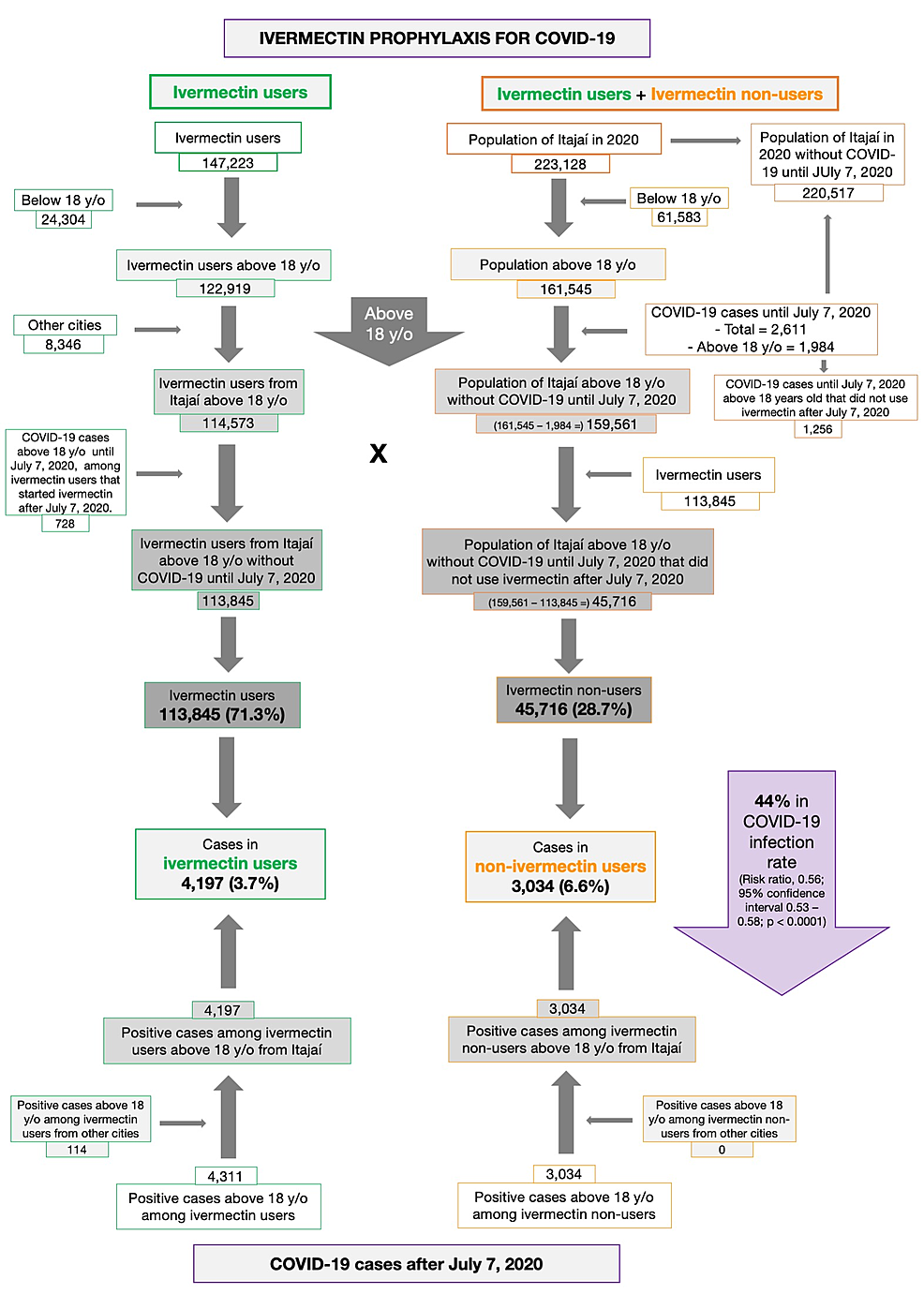
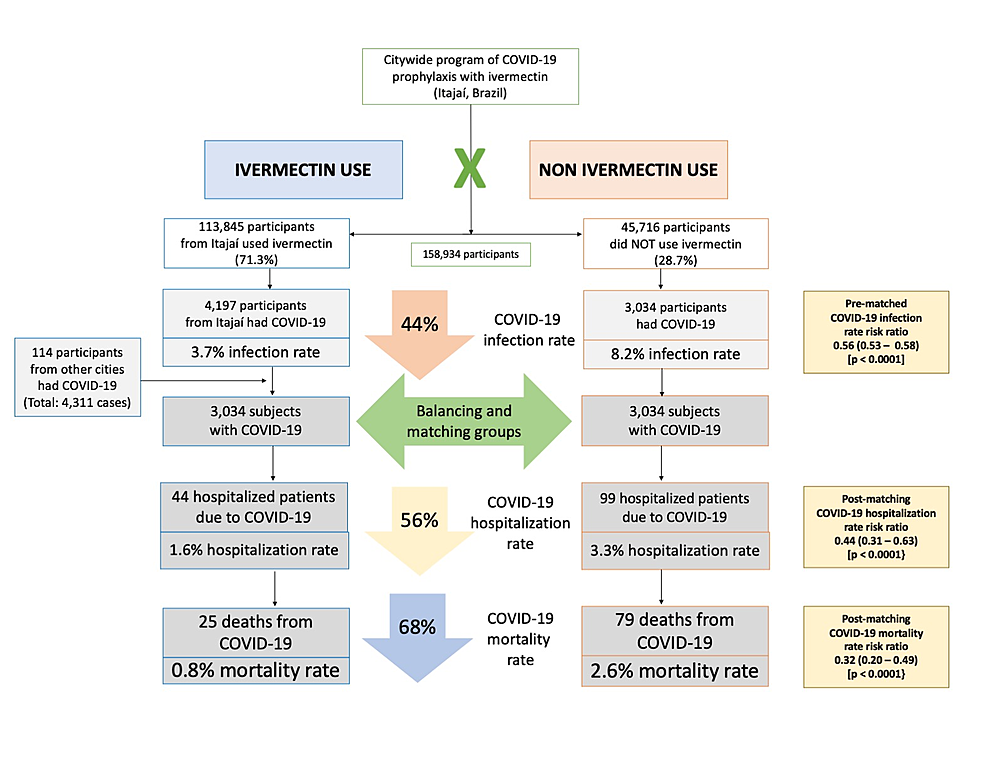
Results: Of the 223,128 citizens of Itajaí considered for the study, a total of 159,561 subjects were included in the analysis: 113,845 (71.3%) regular ivermectin users and 45,716 (23.3%) non-users. Of these, 4,311 ivermectin users were infected, among which 4,197 were from the city of Itajaí (3.7% infection rate), and 3,034 non-users (from Itajaí) were infected (6.6% infection rate), with a 44% reduction in COVID-19 infection rate (risk ratio [RR], 0.56; 95% confidence interval (95% CI), 0.53-0.58; p < 0.0001). Using PSM, two cohorts of 3,034 subjects suffering from COVID-19 infection were compared. The regular use of ivermectin led to a 68% reduction in COVID-19 mortality (25 [0.8%] versus 79 [2.6%] among ivermectin non-users; RR, 0.32; 95% CI, 0.20-0.49; p < 0.0001). When adjusted for residual variables, reduction in mortality rate was 70% (RR, 0.30; 95% CI, 0.19-0.46; p < 0.0001). There was a 56% reduction in hospitalization rate (44 versus 99 hospitalizations among ivermectin users and non-users, respectively; RR, 0.44; 95% CI, 0.31-0.63; p < 0.0001). After adjustment for residual variables, reduction in hospitalization rate was 67% (RR, 0.33; 95% CI, 023-0.66; p < 0.0001).
Conclusion: In this large PSM study, regular use of ivermectin as a prophylactic agent was associated with significantly reduced COVID-19 infection, hospitalization, and mortality rates.
*Source*
*Source*
Cont. from Cureus:
Discussion
This prospective, citywide COVID-19 ivermectin prophylaxis program resulted in significant reductions in COVID-19 infections, hospitalizations, and deaths. The ivermectin non-users were two times more likely to die of COVID-19 than ivermectin users in the overall population analysis. Since groups were compared for the exposure during the same period, in a parallel manner, changes in transmission rates would affect ivermectin users and non-users equally.
The city of Itajaí, in the state of Santa Catarina, Brazil, started a citywide program of prophylaxis with ivermectin in July 2020 as part of several initiatives to reduce the burden of COVID-19. The use of ivermectin was based on the existing literature at that time and on the virtual absence of risks. The National Health System (SUS) functions as full healthcare support to the entire population allowed the city to establish a non-restricted population program. This program included a support structure consisting of a large outpatient clinic located at the Convention Center of Itajaí. This outpatient clinic became the main locale of assistance for COVID-19 patients, supported by multiple public facilities where general practitioners regularly saw patients.
The use of ivermectin was optional unless contraindicated and given upon medical discretion. A structured medical-based program with a medical visit and evaluation of basic demographic characteristics and comorbidities offered ivermectin as optional prophylaxis to those who agreed to participate in this preventive treatment program. Health status was assessed and data were entered prospectively throughout the period of the program, in a fully digitized system provided by the National Health System (SUS). Since the system existed prior to the pandemic, a significant number of the population were already registered with their health information, including past and current diseases, use of medications, and other characteristics. The adaptations made to the SUS for the pandemic preparedness, prior to the initiation of this ivermectin outpatient program, allowed a structured, well-organized collection of the data that monitored any missing values, reinforcing the reliability of the results.
An important conservative bias was present. Major risk factors for severe COVID-19 and mortality due to COVID-19, including aging, diabetes, and hypertension, were more present among ivermectin users, which may have underestimated the benefits of ivermectin as it was demonstrated to be particularly effective in subjects above 49 years old in terms of reduction of absolute risk, which corresponds to the group at the highest risk for COVID-19. This allows the understanding that prophylactic use of ivermectin can be particularly impactful in older subjects. In addition, ivermectin seemed to reduce the exceeding risk of hypertension, T2D, and other diseases.
In accordance with the literature, subjects with higher age, diabetes, and males were less likely to survive (p < 0.05 for all), and only aging remained as an independent risk factor after PSM (p < 0.0001). However, prophylactic ivermectin use appears to mitigate the additional risk of COVID-19 death due to T2D, hypertension, and cardiovascular diseases.
The narrative that using preventive and early treatment therapies will have people relax their caution of remaining socially and physically distanced to allow more COVID-19-related infections is not supported here. These study data demonstrate that the use of preventive ivermectin significantly lowers the infection rate and that benefits outweigh the speculated increased risk of changes in social behaviors. Hence, we can speculate that the prophylactic use of ivermectin could play an important role in the reduction of the pandemic burden.





Join the conversation!
Please share your thoughts about this article below. We value your opinions, and would love to see you add to the discussion!